Menopause. Signs, symptoms and causes
Menopause is the time in the life of a woman when her periods stop, signalling the end of the reproductive function of her body. Both menopause and perimenopause (the transition to menopause) are associated with a number of symptoms that can significantly affect a woman’s quality of life.
Menopausal symptoms can be challenging, and knowing that the process is linked to aging can be difficult to accept. However, as with any other inevitable bodily change, being informed and at peace with what is happening goes a long way towards easing the process and managing symptoms.
“Menopause” is often used as a blanket term for these three stages:
Perimenopause begins when a woman’s ovaries start producing less estrogen and progesterone. Due to this natural decline of reproductive hormones, her periods may fluctuate and her body may undergo a series of changes until her ovaries stop producing eggs, and she has no more periods. Perimenopause typically lasts around 4 years, but can last anywhere from a few months to a decade.
Menopause is confirmed when a woman has had no periods for a year. For the vast majority of women, menopause occurs between 45 and 55 years of age. After menopause comes postmenopause—symptoms usually ease at this point. From start to finish, the whole process can take 2–12 years.
Primary premature menopause happens when the ovaries don’t function normally. It can by caused by genetic disorders (such as Turner syndrome, autoimmune diseases, and primary ovarian insufficiency) that cause accelerated aging of the ovaries. Primary premature menopause can also be caused by medical procedures such as surgical removal of ovaries, pelvic radiotherapy, and anticancer chemotherapy.
Hormone therapy is often recommended at least until menopause would typically occur in order to protect the brain, heart and bones.
In secondary premature menopause, the ovaries function normally, but hormone signals from the brain aren’t getting through. This is usually caused by diseases of the pituitary gland or hypothalamus.
Climacteric disorders
Menopause causes disorders related to estrogen deficiency, called climacteric disorders (or climacteric syndrome), which indicate the endocrine, physical and psychological changes that occur during this period. The severity of these disorders vary from woman to woman.
Climacteric disorders include:
Irregular periods
Periods usually become irregular and/or less frequent. Sometimes they skip a month, or disappear for several months before continuing as usual. The cycle can also shorten for a time before disappearing completely. Pregnancy can occur regardless of menstrual irregularity—if a period has been missed, taking a pregnancy test is recommended for sexually active women, as are regular visits to the doctor during perimenopause, menopause and postmenopause as it can help timely detection of possible health problems that may come with hormonal changes.
Hot flashes
This is the most common manifestation of low estrogen levels. It presents as sudden heat, usually most intense in the face, neck and chest. Hot flashes are sometimes accompanied by intense night sweats, which can be disruptive to the sleep cycle. Several nights of disrupted sleep can result in foggy thinking, irritability, and other symptoms characteristic to menopausal mood swings.
In order to manage hot flashes, one can dress in layers that can be easily removed, have a cold glass of water within reach, or a cooler environment to take refuge in close by. Identifying and subsequently avoiding triggers of hot flashes can also help. Triggers may include hot beverages, caffeine, spicy foods, alcohol, stress, hot weather, even a warm room.
Vaginal dryness and decreased sex drive
Vaginal dryness is uncomfortable, conducive to increased risk infection, and makes sexual intercourse unpleasant, even painful. Understandably, this may reduce desire for sex. Water-based vaginal moisturizers and lubricants as well as topical vaginal estrogen treatments can be used to remedy the condition.
Changes in the skin
Lower levels of sex hormones and aging makes the skin thinner, drier and more fragile. Age spots and areas of darker skin can appear on the face, hands, neck, arms, or chest, especially if a woman has spent a lot of time in the sun without sun protection. Skin cancer and precancerous skin growths are more common as well.
Apply sunscreen with SPF 30 or higher on uncovered parts of your body every day before going outdoors. Regular visits to a dermatologist are also recommended.
Changes in weight distribution and weight gain
Women tend to gain weight as the metabolism slows down, and fat tends to accumulate on the belly rather than the thighs and buttocks.
Breast tenderness, changes in shape
An irregular menstrual cycle can mean unpredictable soreness and tenderness. As estrogen levels drop, the glandular tissue in a woman's breasts shrinks. That causes them to become less dense and more fatty, which can lead to sagging. Wearing a well-fitted, good-quality bra, regular chest exercises and good posture can slow down these changes to some extent.
Urinary incontinence
This mostly takes the form of small, involuntary leaks while sneezing, laughing, coughing or lifting something heavy. As vaginal and urethral tissues slowly lose elasticity, a woman can experience sudden, strong urges to urinate, followed by an involuntary loss of urine. Exercising pelvic floor muscles and using vaginal hormonal ointments may help relieve these symptoms.
Changes in the mind
Going through menopause is just as much of an emotional ordeal as it is a physical one—mood swings, lack of emotional control, emotions parading as other emotions are all part of the “joys” of menopause. Common symptoms include:
Depression
A very common and serious symptom of menopause.
Irritability
Many women find themselves less tolerant and more easily annoyed at things that did not bother them before.
Anxiety
Nervousness and panic attacks are also common during menopause.
Crying episodes
Many menopausal women find themselves weeping over incidents that might not have mattered much before, or over nothing at all. However, crying can reduce stress by providing release of pent-up feelings.
Sleep disorders and insomnia
Insomnia can contribute to mood swings, as it interferes with day-to-day functioning. Insomnia affects 40–50% of menopausal women.
Forgetfulness
Little lapses in memory, like opening the door to a room but being unable to remember what you wanted to do there, are fairly common.
Brain fog, difficulty concentrating
This can be annoying, but if doesn’t hinder your daily life, it should be no cause for concern. Brain fog usually passes as your body adjusts to a new hormonal balance. If the impact is severe, however, see your doctor.
Health concerns
Estrogen promotes the activity of osteoblasts—the cells that produce bone. After menopause, the declining estrogen levels cause a drop in bone density that can render women vulnerable to osteoporosis. The wrists, spine, and hips are particularly affected.
The earlier menopause occurs, the greater the risk of osteoporosis. Other risk factors include being underweight (weight index less than 19 kg/m2), deficits in calcium or vitamin D, hyperthyroidism, having fractured a bone in adulthood, and the intake of certain medications (such as steroids).
Estrogen also plays a protective role against cardiovascular disease, particularly against atherosclerosis. After menopause, this protection is gone. Women who smoke, are overweight, sedentary and have a family history of cardiovascular disease are most at risk.
Heart disease is the leading cause of death in both men and women. If you have any concerns about your cardiovascular health, do not hesitate to speak to your doctor.
Treatment
There are many ways to keep up with and combat menopausal changes in the body. Hormone replacement therapy is one of them. HRT is effective at relieving menopausal symptoms, especially hot flashes and night sweats.
Women who have undergone a total hysterectomy are recommended estrogen-only HRT, which can be a daily tablet, a weekly or twice weekly patch, a daily gel or an implant. To battle vaginal dryness, local estrogens can also be used in the form of vaginal creams, vaginal rings, and pessaries. Most women are prescribed combined HRT (containing both estrogen and progestogen), either as cyclical/sequential HRT, which leads to menstrual bleeding, or combined continuous HRT, which does not. Combined HRT comes in tablet, patch and implant form.
Potential side effects include breast tenderness, headaches, leg cramps, nausea, irritability, depression, and some forms of HRT are associated with an increased risk of blood clots and breast cancer in some women. These may be overcome by a change of dosage, ingredients or route in the HRT prescribed.
There are other healthcare products that can relieve menopausal symptoms, such as tibolone, a synthetic steroid which has the combined effects of estrogen, progesterone, and testosterone. Low-dose antidepressants may also be effective for some.
Phytoestrogens occur naturally in plants, and are able to bind to the body’s estrogen receptors. For this reason, some women eat plants rich in phytoestrogens, but more research is necessary to determine the effectiveness of this approach.
Sage extract is used by women to reduce hot flashes and night sweats during menopause, and has anti-inflammatory properties. Vitamin D and calcium supplements can help prevent osteoporosis.
Exercise regularly. This is crucial both for keeping in shape and hormone regulation. Yoga or tai chi can improve strength and coordination and may help prevent falls that could lead to broken bones. Exercise to strengthen the pelvic and perineum muscles. Kegel exercises can help in case of urinary incontinence.
Psychotherapy can be exceedingly helpful in processing emotional ordeals. Hypnotherapy may decrease the incidence of hot flashes for some menopausal women, and may also improve sleep. Practicing relaxation techniques, such as deep breathing or guided imagery, may help with menopausal symptoms.
Get enough sleep. Avoid caffeine before bed and drinking too much alcohol. It is good to exercise during the day, although not right before bedtime. Maintain a healthy diet. Include a variety of fruits, vegetables and whole grains. Limit saturated fats, oils and sugars. Remember to be social once in a while. Humans are pack animals, people need other people, there is no getting around that. Cherish the connections you have, as friends and loved ones will always make life worth living.
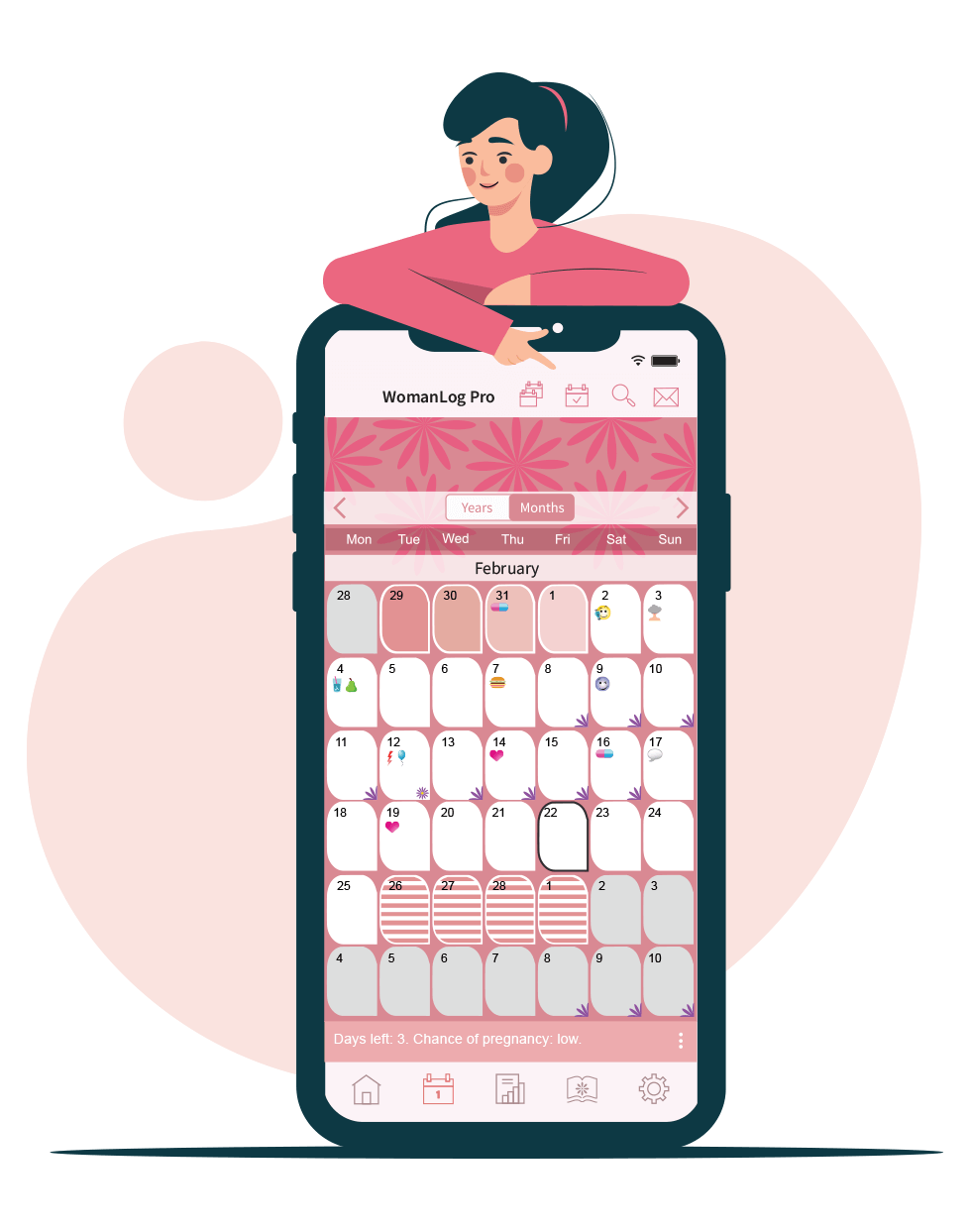
You can track your period and symptoms using WomanLog. Download WomanLog now: